Your Comprehensive Guide to a Type 2 Diabetes Diet Plan: Reclaiming Your Health, One Delicious Bite at a Time
Meta Description: Discover a comprehensive Type 2 Diabetes diet plan that empowers you to take control of your health. Learn practical tips, debunk myths, and find delicious meal ideas to manage blood sugar, boost energy, and live well.
Imagine waking up with more energy, feeling in control of your health, and enjoying delicious food without constant worry. If you’re living with Type 2 Diabetes, or supporting someone who is, the journey can feel overwhelming. But what if the path to a healthier, more vibrant life began right on your plate? This isn’t about deprivation; it’s about empowerment. Get ready to explore a diet plan that’s not just about managing numbers, but about reclaiming your vitality and joy.
Table of Contents
Embracing a New Path – Your Type 2 Diabetes Diet Journey
Receiving a diagnosis of Type 2 Diabetes can bring a whirlwind of emotions. Many individuals experience a sense of loss, fear of endless restrictions, or simply feel overwhelmed by the thought of a “special diet”. It’s a common misconception that managing diabetes means a life devoid of enjoyable food, or that it’s an insurmountable challenge. However, this perspective often overlooks the profound power that dietary choices hold in transforming one’s health.
Instead of viewing a diabetes diet as a punitive measure, consider it a powerful tool for regaining control over your well-being. Strategic food choices can significantly improve how you feel day-to-day, boost your energy levels, and dramatically reduce the risk of serious complications associated with Type 2 Diabetes, such as heart attack, nerve damage, and eye problems. The initial apprehension often stems from a perception of constant limitation, which can exacerbate feelings of distress and make adherence difficult.
By immediately reframing this journey as an opportunity to reclaim vitality and embrace a healthier lifestyle, individuals are better positioned for long-term success. This shift in mindset moves beyond the burden of a diagnosis to highlight the potential for a more fulfilling and healthier life.
Debunking Diabetes Diet Myths: What You Really Need to Know
The world of diabetes management is unfortunately rife with misinformation. Clearing up these common misconceptions is the first step toward building a sustainable and effective Type 2 Diabetes diet plan.
Myth 1: “People with diabetes need to eat special foods.”
Reality: This is perhaps one of the most pervasive myths. The truth is, individuals with diabetes do not require unique, expensive “diabetic” foods. A healthy meal plan for someone managing Type 2 Diabetes is fundamentally the same as healthy eating recommendations for anyone aiming for optimal health. The core principles involve focusing on non-starchy vegetables, limiting added sugars, choosing whole grains over refined ones, and prioritizing whole, unprocessed foods whenever possible.
This emphasis on universal healthy eating helps normalize dietary changes, making individuals feel less isolated or “sick,” and more empowered to integrate these habits into their everyday lives. This normalization is crucial for long-term adherence, as it promotes a broader healthy lifestyle rather than a temporary, restrictive regimen.
Myth 2: “Sugary drinks cause diabetes.”
Reality: While research clearly links the consumption of sugary drinks to an increased risk of Type 2 Diabetes, they are a risk factor, not the sole cause. Developing Type 2 Diabetes is a complex interplay of various factors, including physical activity levels, family history, ethnicity, and age. The American Diabetes Association (ADA) strongly recommends avoiding sugar-sweetened beverages and opting for water whenever possible to help prevent and manage Type 2 Diabetes.
Myth 3: “If you have diabetes, you can’t eat starchy foods like bread, potatoes, and pasta, or any carbs.”
Reality: This is another common fear that can lead to unnecessary deprivation. Starchy foods and carbohydrates can absolutely be part of a healthy Type 2 Diabetes diet plan. The key lies in understanding portion sizes and choosing the right types of carbohydrates. These foods do raise blood glucose, but there is no evidence suggesting that people with diabetes need to avoid carbs entirely.
In fact, balancing carbohydrates with appropriate amounts of protein and healthy fats can help manage blood glucose levels more effectively. The aim is to choose complex carbohydrates, which are digested slower, preventing rapid blood sugar spikes.
Myth 4: “You can never eat sweets or chocolate.”
Reality: This myth often leads to feelings of intense deprivation and can trigger unhealthy binges. The good news is that LOW GLYCEMIC SWEETS and DESSERTS can be enjoyed as part of a healthy meal plan, provided they are consumed in very small portions and reserved for special occasions.
The focus should remain on healthier foods for daily meals, allowing for occasional, mindful indulgences. Working with a registered dietitian nutritionist (RDN) or diabetes care and education specialist (CDCES) can help individuals determine an individualized meal plan that accommodates personal preferences while managing health goals.
Table 1: Low-Glycemic Food Examples For Type 2 Diabetes Diet
| Food Item | Glycemic Index (GI) | Key Characteristic/Note |
| Dark Chocolate (>70% cocoa) | 22 | Rich in flavanols, lower in sugar; supports heart health and insulin sensitivity when consumed in moderation. |
| Cherries | 22 | High in anthocyanins, which may reduce blood sugar and increase insulin production; rich in vitamins and fiber. |
| Late-Ripening Plums | 24 | Low in calories and rich in fiber, beneficial for digestion and heart health. |
| Grapefruit | 25 | Composed of 91% water, rich in vitamin C and soluble fiber; contains naringenin, which may increase insulin sensitivity. |
| Indian Jujube | 25 | Traditionally recognized for its potential in managing high blood sugar levels. |
| Peach | 28 | Good source of fiber, antioxidants, and vitamins; a refreshing low-GI option. |
| Spring Peach | 30 | A less common peach variety, beneficial for reducing the risk of Type 2 Diabetes. |
| Figs | 35 | Contains natural sugars balanced by fiber; best consumed whole and fresh. |
| Pear | 38 | High in water and fiber, helps increase insulin sensitivity and manage blood sugar. |
| Apple | 39 | Rich in vitamin C, soluble fiber, and pectin, which aids in toxin removal and may reduce insulin requirements. |
| Kiwi | 39 | A good source of fiber and vitamins, contributing to stable blood sugar levels. |
| Mountain Tamarind | 40 | Rich in vitamin C and fiber, suitable for daily consumption in a diabetic diet. |
| Strawberries | 41 | Packed with vitamins, antioxidants, and fiber, helping to control diabetes and curb hunger. |
| Orange | 42 | High in fiber and vitamin C, with low sugar content, aiding in blood sugar control and weight management. |
| Blueberries | 53 | High in antioxidants and fiber, contributing to overall health and blood sugar stability. |
Myth 5: “If I take my diabetes medication, I don’t have to worry about my diet and exercise habits.”
Reality: Medication is an important component of diabetes management for many, but it is not a standalone solution. Healthy nutrition and regular physical activity are equally vital and work synergistically with medication to control diabetes effectively. Relying solely on medication without lifestyle adjustments can undermine treatment efforts and increase the risk of complications.
The Pillars of a Type 2 Diabetes-Friendly Diet: Simple Principles for Success
Building an effective Type 2 Diabetes diet plan revolves around a few fundamental principles that prioritize whole, nutrient-dense foods and mindful eating habits.
Focus on Whole, Unprocessed Foods
A consistent theme across reputable dietary guidelines for Type 2 Diabetes is the emphasis on whole, unprocessed foods. These foods are typically higher in fiber, vitamins, and minerals, and naturally lower in added sugars, unhealthy fats, and excessive sodium, which are often abundant in highly processed alternatives. Prioritizing fresh produce, lean proteins, and whole grains forms the foundation of a blood sugar-friendly diet.
Understanding the Balance of Carbohydrates, Proteins, and Healthy Fats
The interplay between macronutrients—carbohydrates, proteins, and fats—is crucial for managing blood sugar levels and overall health.
Carbohydrates: Carbohydrates have the most significant and immediate impact on blood sugar levels because the body breaks them down into sugar. The key is to choose complex carbohydrates found in whole grains, fruits, vegetables, and legumes. These are digested more slowly due to their fiber content, leading to a gradual and more stable release of glucose into the bloodstream, preventing rapid spikes.
Go Complex Carbohydrates For Diabetes
The key is to choose complex carbohydrates found in whole grains, fruits, vegetables, and legumes.
These are digested more slowly due to their fiber content, leading to a gradual and more stable release of glucose into the bloodstream, preventing rapid spikes.

Proteins: High-quality proteins, such as those found in beans, nuts, seeds, fish, poultry, and lean meats, are essential components of a balanced diet. When carbohydrates are consumed alongside protein and healthy fats, the release of glucose into the bloodstream is slowed down. This helps in managing diabetes by preventing sharp blood sugar increases after meals. Protein also contributes to satiety, helping individuals feel fuller for longer, which can naturally reduce overall food intake and support weight management.
Healthy Fats: Not all fats are created equal. Monounsaturated and polyunsaturated fats, found in foods like olive oil, avocado, nuts, seeds, and fatty fish, are preferred choices. These “good” fats are beneficial for heart health and can also contribute to feelings of fullness, further aiding in appetite control. Conversely, saturated and trans fats, often found in processed foods, fatty meats, and full-fat dairy, should be limited due to their potential negative impact on insulin resistance and heart health.

Choose healthy fats like olive oil, avocado, nuts, seeds, and fatty fish.
Avoid fats in processed foods, fatty meat and full-fat dairy
The repeated emphasis on balancing carbohydrates with protein and fat highlights a fundamental principle of blood sugar management. This synergy goes beyond simply avoiding high-carb foods; it’s about optimizing how the body processes nutrients. Protein and healthy fats slow gastric emptying and glucose absorption, leading to more stable blood sugar levels and increased satiety.
This prolonged feeling of fullness can be a powerful ally in reducing cravings and preventing overeating, which are common challenges for many individuals. This understanding moves beyond simple food lists to a more sophisticated appreciation of how foods interact within the body, fostering better adherence and overall well-being.
The Crucial Role of Fiber
Fiber is a superstar nutrient for anyone, but especially for individuals managing Type 2 Diabetes. Abundant in vegetables, fruits, whole grains, and legumes, fiber slows down the digestion process. This slower absorption of nutrients helps to stabilize blood sugar levels, preventing rapid spikes after meals. Additionally, fiber contributes significantly to satiety, helping you feel full and satisfied, which can aid in weight management. Aim for a daily intake of 25-38 grams of fiber.
Eat Foods Rich In Fiber
Fiber is abundant in vegetables, fruits, whole grains, and legumes.
Fiber slows down the digestive process and prevents rapid spikes in blood glucose.
Foods to Savor: Building Your Plate with Confidence
Building a delicious and effective Type 2 Diabetes diet plan means focusing on foods you can enjoy generously, rather than dwelling on restrictions.
Non-Starchy Vegetables: The Cornerstone
Non-starchy vegetables should be the largest component of your meals, ideally filling half your plate. These vegetables are incredibly low in calories and carbohydrates, yet packed with essential vitamins, minerals, and fiber. Excellent choices include green beans, broccoli, spinach, cucumber, romaine lettuce, and bell peppers. They provide bulk and nutrients without significantly impacting blood sugar.
Fruits: Nature’s Sweet Treats (with Mindful Portions)
Fruits are a wonderful source of vitamins, minerals, and fiber. Choose low glycemic fruits. They can be fresh, frozen, or canned (ensuring they are packed in their own juice or water, without added sugar or syrup). While all types of fruit can be part of a healthy diet, portion size is important due to their natural sugar content. Berries, apples, oranges, peaches, and pears are great options.
Whole Grains: Fueling Your Body Steadily
Opt for unprocessed whole grains, which retain their fiber-rich outer shell and inner germ. The fiber in whole grains helps slow digestion, preventing rapid blood sugar spikes and providing sustained energy. Examples include brown rice, quinoa, whole-grain bread and pasta, and oats.
Lean Proteins: Essential for Fullness and Muscle Health
Lean protein sources are vital for building and repairing tissues, and they play a significant role in satiety, helping you feel full and satisfied after meals. Prioritize fish (especially fatty fish like salmon, herring, trout, and sardines, which are rich in heart-healthy omega-3 fatty acids), skinless poultry, lean cuts of meat, eggs, beans, peas, nuts, seeds, and tofu. When preparing proteins, baking, roasting, broiling, or grilling are healthier cooking methods than frying.
Healthy Fats: Good for Your Heart and Overall Well-being
Incorporating healthy fats into your diet is crucial for heart health and can also help with satiety. Focus on monounsaturated and polyunsaturated fats found in olive oil, avocado, nuts, seeds, and fish. These fats contribute to overall well-being beyond just blood sugar management.
While the primary goal of a Type 2 Diabetes diet is blood sugar management, the benefits extend far beyond. The emphasis on nutrient-rich whole foods, healthy fats, and fiber contributes to a holistic improvement in health. For instance, consuming omega-3 fatty acids from fish is directly linked to better heart health , and a diet rich in fruits, vegetables, and fiber can lower the risk of cardiovascular diseases and certain types of cancer.
This broader understanding of the positive impact on long-term health can be a powerful motivator, addressing fears of complications and fostering a sense of reclaiming one’s life.
Foods To Enjoy Versus Limit In Type 2 Diabetes Diet
Table 2 provides a concise, at-a-glance summary of food choices, designed to be a practical guide for quick decisions during meal planning or grocery shopping.
Table 2: Foods to Enjoy vs. Foods to Limit (Quick Reference)
| Foods to Enjoy | Foods to Limit/Avoid |
| Non-Starchy Vegetables: Broccoli, spinach, green beans, bell peppers, cucumber, lettuce | Processed Carbs/Refined Grains: White bread, white rice, white pasta, sugary cereals |
| Fruits: Apples, berries, oranges, peaches, pears (fresh/frozen/canned in own juice) | Added Sugars/Sugary Drinks: Soda, juice, sports drinks, candy, cakes, cookies, sweetened fruit, regular jam |
| Whole Grains: Brown rice, quinoa, whole-grain bread/pasta, oats, millet, buckwheat | Unhealthy Fats: Saturated fats (bacon, fatty meats, full-fat dairy, butter, coconut/palm oil), Trans fats (“partially hydrogenated oils,” fried foods, processed snacks) |
| Lean Proteins: Fish (salmon, sardines), skinless poultry, lean meat cuts, beans, lentils, tofu, eggs, nuts, seeds | High Sodium Foods: Canned soups, microwave meals, pickles, sauerkraut, chips |
| Healthy Fats: Olive oil, avocado, nuts, seeds | Processed Meats: Deli meats, hot dogs, fried proteins |
| Dairy (low-fat): Skim/1% milk, low-fat yogurt/cheese |
Foods to Limit: Navigating the “No-Go” Zones

Avoid These Foods Like Covid
- Refined Carbohydrates and Processed Foods.
- Added Sugars and Sugary Beverages
- Unhealthy Fats (Saturated and Trans Fats).
- High-Sodium Foods
Understanding which foods to limit is as important as knowing what to embrace. These categories often contribute to rapid blood sugar spikes, unhealthy weight gain, and increased risk of complications.
Refined Carbohydrates and Processed Foods
These foods, such as white bread, white rice, sugary cereals, and many packaged snacks, are quickly broken down into sugar, leading to rapid blood sugar spikes. They offer minimal nutritional value and fiber, making them less satisfying and potentially contributing to overeating.
Added Sugars and Sugary Beverages
A significant contributor to high blood sugar and unhealthy weight gain, added sugars are found in soda, fruit juices with added sugar, sports drinks, candy, cakes, cookies, and many sweetened desserts. The American Heart Association recommends limiting added sugar intake to less than 6 teaspoons (25 grams) per day for women and 9 teaspoons (36 grams) per day for men. Replacing sugary drinks with water is a simple yet impactful change.
Unhealthy Fats (Saturated and Trans Fats)
Certain fats can increase insulin resistance and negatively impact heart health, a critical concern for individuals with Type 2 Diabetes. Saturated fats are found in fatty meats, full-fat dairy products, butter, and tropical oils like coconut and palm oil. Trans fats, often listed as “partially hydrogenated oils” on food labels, are particularly harmful and should be avoided. Opt for healthy cooking methods like baking, roasting, broiling, or grilling instead of frying.
High-Sodium Foods
Excessive sodium intake can raise blood pressure, a common co-morbidity with Type 2 Diabetes. Limiting intake of high-sodium foods like canned soups, microwave meals, pickles, sauerkraut, and chips is important. The ADA recommends limiting sodium intake to under 2,300 mg per day.
A significant challenge in navigating a healthy diet is the prevalence of “hidden” unhealthy ingredients in processed foods. Sugars, sodium, and unhealthy fats are often present in seemingly innocuous items. This highlights the importance of developing critical literacy in reading food labels and understanding that claims like “sugar-free” don’t necessarily mean carbohydrate-free or healthier overall.
This goes beyond simple dietary rules; it empowers individuals to make informed choices in a complex food environment, fostering a deeper understanding of what they consume. Over time, as individuals reduce their intake of added sugars, taste buds adapt, and cravings for overly sweet foods naturally diminish.
Crafting Your Personalized Meal Plan: Practical Strategies for Daily Living
Developing a personalized meal plan for Type 2 Diabetes doesn’t have to be complicated. Simple, visual tools and practical strategies can make healthy eating an enjoyable and sustainable part of your daily routine.
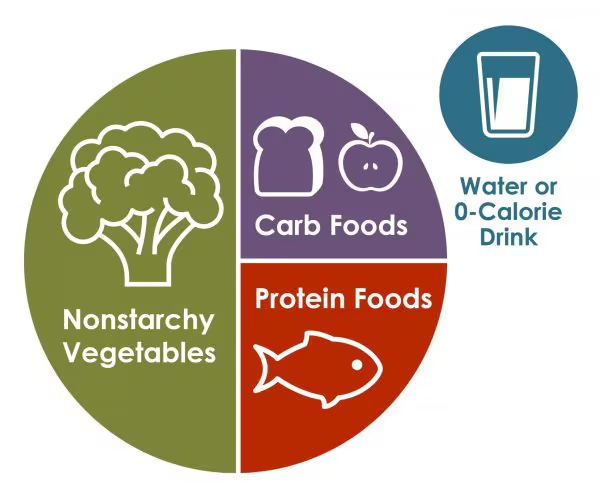
The “Plate Method”: A Simple Visual Guide for Balanced Meals
The Plate Method is a widely recommended and easy-to-understand visual guide for balancing your meals. It simplifies portion control and food group balance, making healthy eating intuitive and less overwhelming, especially for those newly diagnosed. This visual simplicity helps reduce the cognitive load often associated with managing a chronic condition, making long-term adherence more achievable.
Table 3: The Diabetes Plate Method (Visual Guide)
This table illustrates the recommended proportions for a balanced meal using a standard 9-inch plate.
| Section of Plate | Food Group | Examples |
| 1/2 Plate | Non-Starchy Vegetables | Broccoli, spinach, green beans, bell peppers, cucumber, lettuce |
| 1/4 Plate | Lean Protein | Chicken, fish, beans, tofu, eggs, lean meat |
| 1/4 Plate | Healthy Carbohydrates | Brown rice, whole-grain pasta, quinoa, fruit |
Understanding Carbohydrate Counting
For some individuals, particularly those on mealtime insulin, a more precise approach like carbohydrate counting may be beneficial. This involves tracking the grams of carbohydrates consumed at each meal and snack. Since carbohydrates have the biggest impact on blood sugar levels, understanding their quantity allows for more accurate medication dosing and tighter blood sugar control. Your healthcare professional or a registered dietitian can help determine if carbohydrate counting is appropriate for your specific needs.
Sample Daily Meal Plan: Ideas for Breakfast, Lunch, Dinner, and Snacks
Consistency in meal timing and carbohydrate intake is crucial for maintaining stable blood sugar levels. Irregular eating patterns or skipping meals can lead to unpredictable blood sugar spikes or dangerous lows, especially for those on medication. Establishing a routine for meals and snacks provides a framework for consistent blood sugar control, contributing to improved energy and fewer “highs and lows” throughout the day.
Table 4: Sample 1-Day Type 2 Diabetes Meal Plan
This sample plan provides concrete, actionable examples of how to structure meals and snacks throughout the day, demonstrating the application of the Plate Method and general dietary principles.
| Meal | Example Meal Idea | Approximate Carb Count |
| Breakfast | Egg sandwich (whole wheat English muffin, 1 egg), 1/2 banana, 1 cup low-fat milk | 30g |
| Lunch | Turkey sandwich (2 slices whole wheat bread, 3 oz turkey, 1 tbsp mustard), 1 cup baby carrots with 1 tbsp ranch, 10 small grapes, 1 cup low-fat milk | 30-40g |
| Afternoon Snack | 6 whole wheat crackers, 1 oz string cheese | 15g |
| Dinner | 3 oz chicken breast, 1 cup whole wheat pasta, 1/2 cup green beans, 1 cup low-fat milk | 30-40g |
| Note: Carb counts are approximate and individual needs may vary. Always consult with your healthcare team for personalized guidance. |
Portion Control: Mastering the Art of Mindful Eating
Beyond what you eat, how much you eat profoundly impacts blood sugar levels and weight management. Simple strategies can make a big difference:
- Use smaller plates, such as 10-inch plates instead of 12-inch ones, to help manage portion sizes.
- Avoid “second helpings”.
- Practice mindful eating by taking sips of your drink between bites to slow down your eating pace.
- Aim to limit meals to about 30 minutes.
- Use everyday objects as visual guides for portions (e.g., a deck of cards for meat, a fist for cooked pasta/rice).
Eating Out and Special Occasions: Strategies for Staying on Track
Social events and dining out can present unique challenges, but with a little planning, you can navigate them successfully. The key is proactive planning, which reduces stress and significantly increases the likelihood of adherence in challenging social situations. This foresight fosters a sense of control and adaptability, crucial for a sustainable lifestyle transformation.
- Before you go, look up the restaurant’s nutrition information and menu online.
- Plan what you’d like to eat and how it fits into your meal plan.
- Consider sharing a meal or a side dish to manage portions.
- Don’t hesitate to ask for smaller portions, such as a lunch or kid-sized option.
- Request sauces and dressings on the side, and ask for no added salt.
- Prioritize fresh fruits and vegetables, and grilled or baked proteins without heavy sauces or cheese.
- When it comes to sweets, remember they can be enjoyed in very small portions for special occasions, as discussed earlier.
- If you choose to drink alcohol, limit the amount and always have it with a meal. Opt for lower-carb alcoholic beverages like light beer or dry wines, and use sugar-free mixers.
Beyond the Plate: Holistic Well-being with Type 2 Diabetes
Managing Type 2 Diabetes effectively extends beyond just dietary changes. A holistic approach that integrates physical activity, emotional well-being, and professional support creates a powerful synergy for long-term health.
The Synergy of Diet and Physical Activity
Exercise is a powerful partner to diet in managing Type 2 Diabetes. Regular physical activity helps maintain blood sugar levels within a healthy range, burns calories, improves blood flow, and significantly boosts mood. Aim for at least 30 minutes of moderate-intensity physical activity most days of the week. Even short walks after meals can be incredibly effective at preventing blood sugar spikes.
Both aerobic exercise (like walking, jogging, swimming, or cycling) and resistance training (strength training) offer distinct benefits. Aerobic exercise helps lower blood glucose levels during and after activity by using glucose in the blood for energy, much like a sponge soaking up water. Resistance training, by increasing muscle size, creates more storage space for glucose in cells, burns more energy even at rest, and improves overall physical function. This understanding of how exercise directly impacts blood sugar levels provides a tangible and immediate benefit that can be highly motivating.
Weight Management: Small Changes, Big Impact
If you are overweight, even modest weight loss can yield significant health improvements. Losing as little as 5-10% of your body weight can lead to substantial improvements in blood sugar levels, A1C, cholesterol, and blood pressure. For instance, a 5-10% weight loss has been shown to lower A1C by an average of 0.5%. This emphasizes that achievable, modest goals can lead to significant positive outcomes, making the journey feel less daunting and more motivating. The more weight you lose, the greater the health benefits.
Addressing Emotional Challenges: Stress, Anxiety, and Diabetes Distress
Living with a chronic condition like Type 2 Diabetes can take an emotional toll. Individuals with diabetes are two to three times more likely to experience depression and approximately 20% more likely to have anxiety compared to those without diabetes. There is a critical bidirectional relationship between mental health and diabetes management: untreated mental health issues can worsen diabetes control, and conversely, the challenges of managing diabetes can exacerbate mental health problems. Stress hormones, for example, can cause unpredictable fluctuations in blood sugar levels.
A common experience is “diabetes distress,” where individuals feel discouraged, worried, or simply tired of the daily demands of diabetes care. This can lead to neglecting self-care habits. Recognizing this connection is vital. If one aspect improves, the other often follows. Solutions include seeking professional help from a therapist, diabetes educator, or endocrinologist who understands chronic health conditions. Engaging in physical activity, practicing relaxation exercises like meditation or yoga, and prioritizing self-care activities can also significantly help manage stress and anxiety.
The Power of Your Support Team: Doctors, Dietitians, and Educators
While general guidelines are helpful, the reality is that “there isn’t one eating plan that prevents or manages diabetes that anyone can use”. Effective Type 2 Diabetes management requires an individualized approach tailored to personal preferences, lifestyle, cultural background, and other co-existing health conditions. This underscores the critical role of personalized professional guidance.
Your healthcare team—including your doctor, a registered dietitian (RDN), and a diabetes care and education specialist (CDCES)—is your most valuable partner. A dietitian can help you make healthy food choices, plan meals, and develop strategies for changing habits. They can also provide practical advice for navigating challenging situations like eating out or understanding complex nutrition information. This expert tailoring ensures that your plan is not only effective but also sustainable, preventing frustration from generic advice and leading to long-term adherence.
Your Transformation Story: Goals Achieved, Life Reclaimed
The journey of managing Type 2 Diabetes through diet is one of continuous learning and adaptation, but it is also a journey of incredible transformation. Real-life experiences demonstrate the profound impact of taking control through dietary changes.
Consider Roger Hare, who, despite initial denial and a moment of overwhelm at the grocery store, transformed his health. Through a strict low-carb diet and exercise, he lowered his A1C from 6.7 to 6.3 and his cholesterol from 222 to 95. His motivation was deeply personal: wanting to see his daughter grow up and walk down the aisle. This kind of relatable narrative provides more than just information; it offers hope, inspiration, and a sense of shared experience. Connecting with the emotional journey of others can be a powerful catalyst for sustained behavioral change, turning abstract health goals into tangible, deeply personal motivations.
The goal is to keep blood sugar levels within your target range to delay or prevent serious complications. Achieving an A1C level below 7% is a primary objective to significantly reduce the risk of long-term complications. By focusing on small, sustainable changes, you can achieve remarkable results. Remember, even modest weight loss of 5-10% of your body weight can lead to significant improvements in blood sugar, cholesterol, and blood pressure. Establishing a regular schedule for meals and snacks further aids in stabilizing blood sugar levels.
Your plate is a powerful tool. By embracing these principles, seeking professional guidance, and committing to sustainable lifestyle changes, you can reclaim your vitality, manage your Type 2 Diabetes effectively, and live a fuller, healthier life.
Frequently Asked Questions (FAQ)
What is a good diet for people with diabetes?
There isn’t one single “best” diet for everyone with diabetes. The most effective approach is generally a healthy eating plan that focuses on whole, unprocessed foods, a balance of macronutrients (carbohydrates, proteins, healthy fats), and plenty of fiber. Personalization based on individual preferences, lifestyle, and other health conditions is key.
What foods should someone with diabetes avoid?
Individuals with Type 2 Diabetes should limit or avoid processed foods, fried foods, foods high in saturated and trans fats, very salty foods, and foods and drinks with added sugar. These foods can cause rapid blood sugar spikes and contribute to other health complications.
What are the three rules of a diabetic diet?
While not rigid “rules,” three key areas to focus on for managing blood glucose levels are: what you eat (prioritizing healthy, whole foods), when you eat (maintaining regular meal times), and how much you eat (practicing mindful portion control).
Can people with diabetes eat starchy foods or carbs?
Yes, starchy foods and carbohydrates can be part of a healthy Type 2 Diabetes diet plan, but moderation and mindful portion sizes are crucial. Focus on high-fiber, complex carbohydrates like whole grains, fruits, and non-starchy vegetables, and balance them with protein and healthy fats to help stabilize blood sugar levels.
How can someone lower their A1C levels through diet?
Lowering A1C levels through diet involves consistent healthy eating habits, diligent portion control, eating regular meals, spreading carbohydrate intake throughout the day, increasing fiber consumption, and achieving modest weight loss. These combined efforts contribute to more stable blood sugar over time.
Is intermittent fasting a good option for people with diabetes?
While some studies suggest potential benefits, such as A1C reduction with specific intermittent fasting patterns like the 5:2 meal replacement plan , it is not yet clearly established as a universally good option for all individuals living with diabetes. It is crucial to consult your healthcare team before attempting intermittent fasting or any significant dietary change.
Do I need to check my blood sugar every day if I change my diet?
Yes, regularly tracking your blood sugar is important to understand how different foods and meals affect your individual glucose levels. Checking your blood sugar before and approximately two hours after meals can provide valuable information about the impact of your dietary choices. Your healthcare team will advise on the frequency of monitoring.
References
American Diabetes Association. (n.d.). About Diabetes: Diabetes Myths. Retrieved from https://diabetes.org/about-diabetes/diabetes-myths
American Diabetes Association. (n.d.). Eating for Diabetes Management. Retrieved from https://diabetes.org/food-nutrition/eating-for-diabetes-management
American Diabetes Association. (n.d.). Get to Know Carbs. Retrieved from https://diabetes.org/food-nutrition/understanding-carbs/get-to-know-carbs
American Diabetes Association. (n.d.). Sharing My Story: Roger Hare. Retrieved from https://diabetes.org/blog/sharing-my-story-roger-hare
American Diabetes Association. (n.d.). Weight Management. Retrieved from https://diabetes.org/health-wellness/weight-management
Better Health Channel. (n.d.). Diabetes and healthy eating. Retrieved from https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/diabetes-and-healthy-eating
Centers for Disease Control and Prevention. (n.d.). Living with Diabetes: Mental Health. Retrieved from https://www.cdc.gov/diabetes/living-with/mental-health.html
Cleveland Clinic. (n.d.). Type 2 Diabetes. Retrieved from https://my.clevelandclinic.org/health/diseases/21501-type-2-diabetes
GoodRx. (n.d.). Type 2 Diabetes Diet Plan of Foods Diabetics Can Eat. Retrieved from https://www.goodrx.com/conditions/diabetes-type-2/type-2-diabetes-diet-plan-of-foods-diabetics-can-eat
Hopkins Medicine. (n.d.). Managing Diabetes: Six Healthy Steps With the Most Benefit. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/managing-diabetes-six-healthy-steps-with-the-most-benefit
Hopkins Medicine. (n.d.). Prediabetes Diet. Retrieved from https://www.hopkinsmedicine.org/health/wellness-and-prevention/prediabetes-diet
Mayo Clinic. (n.d.). Diabetes Diet: Create Your Healthy-Eating Plan. Retrieved from https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-diet/art-20044295
Mayo Clinic. (n.d.). Diabetes Management: How Lifestyle, Daily Routine Affect Blood Sugar. Retrieved from https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-management/art-20047963
Mayo Clinic. (n.d.). How to Live Well With Diabetes. Retrieved from https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/how-to-live-well-with-diabetes
Mayo Clinic. (n.d.). Type 2 Diabetes: Diagnosis and Treatment. Retrieved from https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/diagnosis-treatment/drc-20351199
Mayo Clinic. (n.d.). Type 2 Diabetes: Symptoms and Causes. Retrieved from https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193
Medical News Today. (n.d.). What is a good diet for type 2 diabetes?. Retrieved from https://www.medicalnewstoday.com/articles/324416
MedlinePlus. (n.d.). Diabetes Diet. Retrieved from https://medlineplus.gov/ency/article/007429.htm
Mount Sinai. (n.d.). Diabetes Diet. Retrieved from https://www.mountsinai.org/health-library/report/diabetes-diet
NHS. (n.d.). Type 2 diabetes: Treatment. Retrieved from https://www.nhs.uk/conditions/type-2-diabetes/treatment/
Sugarfit. (n.d.). Type 2 Diabetes Diet. Retrieved from https://www.sugarfit.com/blog/type-2-diabetes-diet/
Sutter Health. (n.d.). Diabetic Meal Plan. Retrieved from https://www.sutterhealth.org/health/diabetic-meal-plan
University of Iowa Health Care. (n.d.). Meal Planning for Type 2 Diabetes. Retrieved from https://uihc.org/childrens/health-topics/meal-planning-type-2-diabetes
University of Massachusetts Medical School. (n.d.). Success Stories. Retrieved from https://www.umassmed.edu/dcoe/diabetes-care/success-stories/
WebMD. (n.d.). Diabetic Food List: Best & Worst Foods. Retrieved from https://www.webmd.com/diabetes/diabetic-food-list-best-worst-foods
WebMD. (n.d.). Diabetes: Healthy Quick Meals. Retrieved from https://www.webmd.com/diabetes/diabetes-healthy-quick-meals
